Bariatric-surgery or weight-loss surgery has been shown to help improve or reverse many obesity-related conditions such as Type 2 diabetes, high blood pressure, heart disease, and more. Dr. Jaydeep Palep, Bariatric Surgeon at Nanavati Hospital, provides in-depth information on how it can have a positive effect on the health of obese individuals.
Bariatric surgery has emerged as a treatment option for obesity and is increasingly recognized to have benefits for glycemic management in patients with pre-existing Type 2 diabetes. How does bariatric surgery cause Type 2 diabetes to go into remission?
Bariatric surgery is indeed very beneficial for Type II Diabetes Mellitus. Numerous studies conducted all over the world have found that diabetes remission starts even before the weight loss kicks in. After surgery, food tends to reach the small intestine faster than usual. This causes multiple insulin like hormones to be released, which help in lowering blood sugar levels. This effect may persist for 10 to 15 years after surgery, which essentially means no or minimal medications for diabetes may be needed after surgery for 10 to 15 years.
What are the different types of bariatric surgery?
Bariatric surgery is broadly classified as –
- Restrictive
- Malabsorptive or both.
The most commonly performed surgery is the sleeve gastrectomy, which is a restrictive procedure. The other surgeries include traditional Roux-en-Y Gastric Bypass, Mini Gastric Bypass and Sleeve Gastrectomy with Duodenojejunal Bypass. All of these are restrictive and malabsorptive surgeries. In addition to these, there are some more procedures, but their efficacy in the Indian population is not yet well established.
What are other beneficial effects of bariatric surgery in diabetic patients?
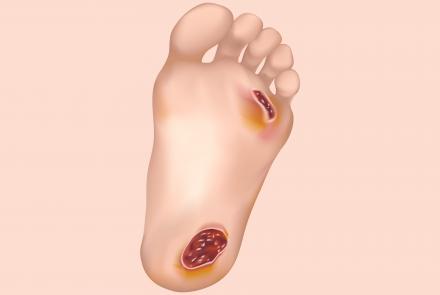
By giving us remission of Diabetes, this surgery automatically prevents all complications of Diabetes, thus saving your kidneys, eyes, heart and limbs. In addition to this, it also helps in lowering of blood pressure in hypertensive patients, resolution of obstructive sleep apnea, better control of thyroid disorders and Polycystic ovary syndrome (PCOS), improved fertility rates, and an overall positive socioeconomic effect.
What is the success rate of bariatric surgeries?
Success in Bariatric surgery is traditionally defined as losing more than 50 % excess weight. More than 90% of the patients achieve this target. Long term weight maintenance happens when the patient sticks to a healthy lifestyle post-surgery.
Is bariatric surgery more effective than drug therapy in the management of diabetes?
Yes, many studies conducted in multiple countries have proven that surgery is more effective at controlling blood sugar levels as compared to medications alone. This is why, today bariatric surgery has been renamed metabolic surgery.
Besides diabetes, bariatric surgery is believed to be effective in controlling other diseases such as PCOS and reducing risk of Cancer. What has been your experience?
Morbid obesity is linked to multiple diseases other than Diabetes, such as Hypertension, Obstructive sleep apnea, PCOS, hypothyroidism, liver disease etc. Hence, it stands to reason that as the patient loses weight, these conditions improve and the risk of acquiring diabetes or cancer of the breast, ovary and colon at a later stage in life drastically reduces.
Is bariatric surgery safe and cost-effective?
Bariatric surgery is as safe as any other surgical procedure, for example, undergoing a hernia or an appendix surgery. Overall, it is cost effective, because after this surgery you are less likely to need any further hospitalisations or surgeries for diseases caused by morbid obesity.
Bariatric Surgery Common Risks
- Acid reflux
- Chronic nausea and vomiting
- Dilation of oesophagus
- Obstruction of stomach
- Inability to eat certain foods
- Weight gain or failure to lose weight
Who is not an ideal candidate for a bariatric surgery?
Any patient who is below a BMI of 37 without any comorbidities is not a candidate for surgery. In addition, patients below a BMI of 32 even with comorbidities are, strictly speaking, not candidates for surgery. In certain cases, where the BMI is above 27.5 and the patient has uncontrolled diabetes even with maximal medical therapy, we may consider surgery, as per the International Diabetes Federation guidelines.
What are the management strategies to be followed after a bariatric surgery?
Post-surgery, the patient's motivation and will power is the key to long term success. The patient has to adopt a healthy lifestyle, eat a protein rich diet and exercise regularly. These are simple changes which every human needs to follow anyway.
Bariatric Surgery Long-Term Risks
- Dumping syndrome, leading to nausea and dizziness
- Hernias
- Low blood sugar
- Malnutrition
- Vomiting
- Ulcers
- Bowel obstruction
Has bariatric surgery become popular in India? Could you give us some statistics?
The popularity of bariatric surgery has definitely grown globally and also in India. This growth is absolutely justified because morbid obesity is now a pandemic, and India now ranks third in the world in terms of obese population. Surgical numbers have been increasing in proportion to the number of morbidly obese people, and have almost tripled over the last 4 to 5 years.